We are on the cusp of a cure
Dr Paul Mulholland
The treatment approach for glioblastoma has not changed for decades, so outcomes remain dismal. But there is another way.
There are drugs that are being used every day around the world to treat and cure other cancers. We can use these drugs, and in particular immunotherapy, to help treat glioblastoma.
We have seen the ongoing success with Ben Trotman and Professor Richard Scolyer after their treatment with immunotherapy. The big difference with Ben and Richard is that they were treated with immunotherapy before embarking on other treatments. The time before those treatments is when the body is able to generate an immune response to fight the tumour.
This approach works but we need to run more trials to prove it to the world. That means drugs from the pharmaceutical industry and money. Hence the fundraising efforts started by Margaret and continued by Siobhain.
As soon as we satisfy the regulatory authorities, treatment can then be rolled out to save the lives of people diagnosed with the illness that took Margaret from us.
From the bottom of my heart, thank you. We can win Margaret’s final campaign.
The Glioblastoma Campaign has five steps to finding a cure
A target of getting 200 glioblastoma patients into clinical trials each year on a drug that has the potential to change the course of the disease.
The NHS must work towards delivering clinical trial options to patients with drugs that are aimed to change the natural history of glioblastoma.
The pharmaceutical industry should recognise their responsibility to support glioblastoma and other left-behind cancers by making their drugs available for clinical trials.
The NHS should ensure that every neuro-oncology multidisciplinary team has a medical oncologist who is a core member and is required to attend meetings to discuss patients. Brain tumour patients must not be left in a corner of the ward, there must be specialists arguing for them.
The NHS should require that every doctor training to be a medical oncologist should go through mandatory training in medical oncology specific to primary brain cancer.
About Glioblastoma
About Glioblastoma
Glioblastoma is the most common form of brain cancer in adults. It is extremely aggressive and has no cure. The current treatment for glioblastoma was introduced more than 20 years ago and little changed, until now, with the Win-Glio Programme.
Cancer Research UK calls glioblastoma a ‘cancer of substantial unmet need’.
With no cure for glioblastoma, the survival rate is less than a year.
It is the most common type of brain cancer in adults, accounting for approximately half of all cancerous primary brain tumours.
About 3,000 new cases are diagnosed in the UK annually.
The current treatment protocol delivers a modest improvement in survival rates of up to 15 months.
Despite killing more children and adults under the age of 40 than any other cancer, brain tumours receive just 1% of the national spend on cancer research.
The Win-Glio Programme
The Win-Glio Programme of clinical trials improves the effectiveness of cancer drugs by using them alongside drugs that modulate the immune system.
Both types of drugs have already been licensed or are in clinical development.
It’s known how these drugs work. It’s known what they do to tumours, what the correct dose is, and the potential side-effects. This isn’t starting from scratch.
Immunotherapy has already been successfully used with melanoma (skin cancer) patients. Because melanoma shares similarities to glioblastoma brain cancer there is every chance these successes can be replicated.
The Win-Glio programme, launched at the end of 2023, is developing its first trial for early 2025. It will involve ten patients who are due to have surgery for glioblastoma. These patients will receive immunotherapy drugs to target the glioblastoma cancer. There will be multiple trials, each using different immunotherapy drugs. A significant response rate in one of the cohorts of patients will allow further patients to be enrolled into this group to give a statistically significant number of patients for further analysis.
The Win-Glio Programme is led by Dr Paul Mulholland. Paul is a medical oncologist who exclusively treats brain cancer. He is a consultant at University College Hospital, the National Hospital for Neurology and Neurosurgery (part of UCLH).
A new approach to treating Glioblastoma
Learning from melanoma success
Immunotherapy drugs have transformed the survival of people living with melanoma. And melanoma shares similarities to glioblastoma brain cancer. Brain cancer cells and skin cancer cells have similar genetic changes. This may be because brain and skin cells share the same embryonic development.
In about half of cases, the melanoma cells have a particular genetic mutation, called a BRAF mutation, and this causes the melanoma cells to divide and grow. These patients respond well to molecularly targeted therapies. There are a group of brain tumour patients who also have the same BRAF gene mutation as the melanoma patients who also respond well to the same molecularly targeted therapies.
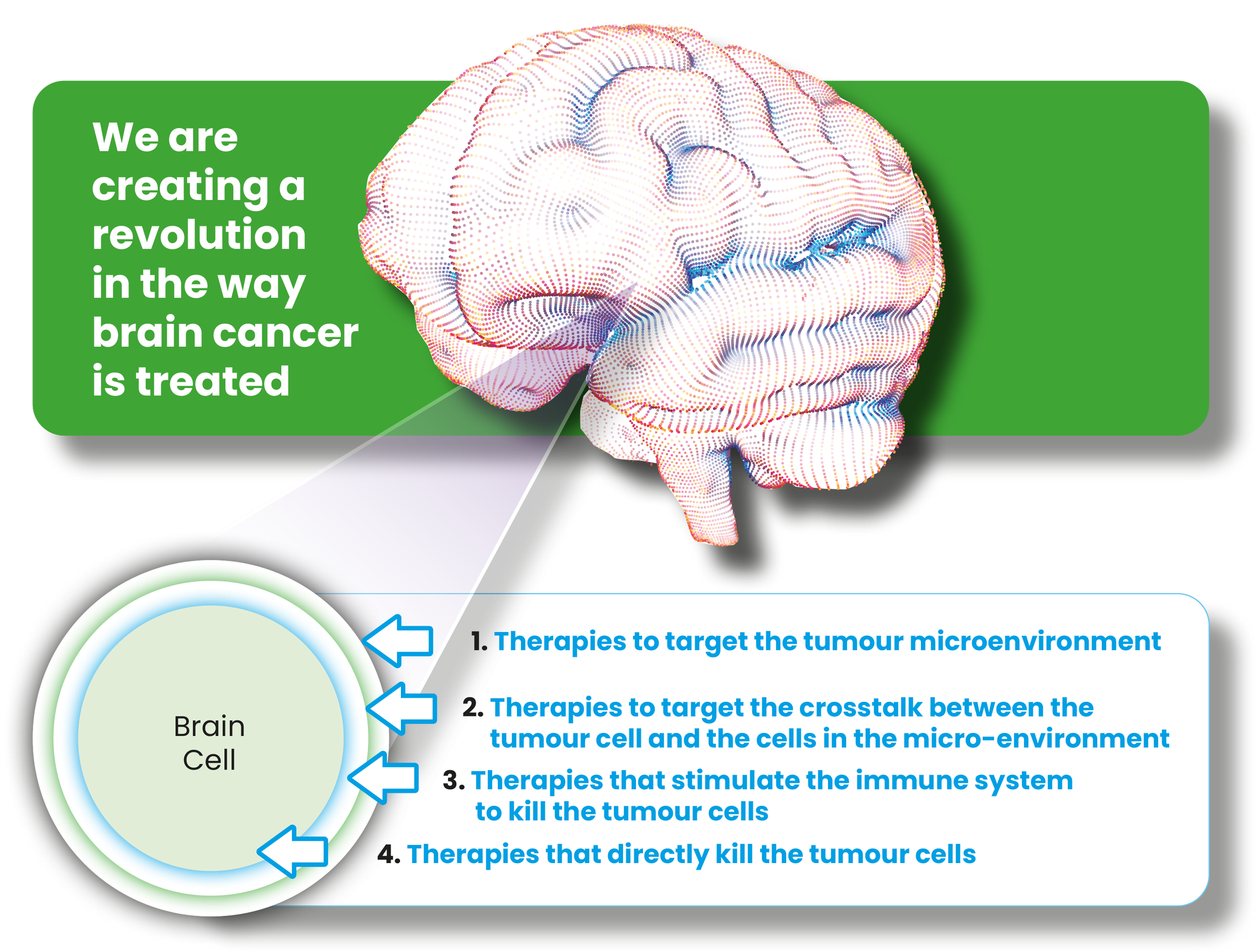
However, in brain cancer there is a tumour mass which contains the glioblastoma cancer cells but also a microenvironment of other cells around it that support and protect the glioblastoma cancer cells preventing the immunotherapy working. This microenvironment can be targeted to stop it protecting the brain cancer cells.
The Win-Glio trial programme will use drugs that interfere with the microenvironment protection for the cancer cells and give immunotherapy drugs to strengthen the immune response and attack the glioblastoma cancer cells.
Immunotherapy puts Glioblastoma into Remission
Something remarkable happened in Australia and it is being closely followed in the UK.
Professor Richard Scolyer, co-director of the Melanoma Institute Australia and a pioneer of life-changing immunotherapy treatments for skin cancer patients, was himself diagnosed with a glioblastoma a year ago and applied his own immunotherapy treatment to himself, consulting as he did so with the UK’s leading expert in this field, Dr Paul Mulholland.
Before surgery to remove what was visible of the tumour, Prof Scolver took immunotherapy drugs designed to prime his immune system to recognise and attack the cancer cells. Then he also took a personalised vaccine, built around markers specific to the tumour, designed to induce an immune response.
The idea was that once the cancer was removed, he could have his body trained to fight it, to make it harder for it to re-establish itself. He doesn’t yet know if the cancer is defeated. But he does know that his tumour still hasn’t returned, at a stage when most of those with the same diagnosis are already dead.
“I’m the best I have felt for yonks,” he said, adding that he’s back to exercising every day – which for him often means a casual 10-mile jog.
My treatment success
by Ben Trotman, West Sussex, UK
2022 was shaping up to be a pretty great year – I got engaged to the love of my life, celebrated my 40th birthday and started an exciting new job. The future was looking bright, with plans for our wedding, buying our first house together and starting a family all firmly on the horizon.
Without warning, in October 2022, I experienced a seizure whilst out shopping. Blue lights, A&E, needles, scans and all manner of tests followed. This was a terrifying time with a wait of 4 weeks to see an NHS consultant.
In desperation for help, my fiancé contacted the National Hospital for Neurology and Neurosurgery. As I was fortunate enough to have health insurance through my employer, we hoped that we might be able to access a specialist at the hospital quickly. I was offered an appointment with Dr Paul Mulholland the following day and finally told that glioblastoma was the most likely diagnosis. This was devastating news as we knew what a terrible prognosis it carried from weeks of frantic googling. We were given a glimmer of hope, however, as we learned that I could be eligible for a clinical trial in the NHS. Given how dreadfully bleak the outcomes for glioblastoma with standard treatment are, we were incredibly grateful for the opportunity to try something different.
Prior to commencing the standard combined chemo-radiotherapy treatment, I received a trial dose of immunotherapy – a drug to boost my immune response and improve the efficacy of subsequent treatments. For now, it seems to be having the effect we had so hoped for – it’s almost two years on from my diagnosis and my most recent scans have shown no detectable tumour. Given how well I am currently, and how thrilled we are to be able to make the most of this time, we were horrified to learn that no other patients benefitted from the trial which I took part in, because not a single other person was referred. I am delighted to see the success that Professor Scolyer has had in Australia with his own treatments using these drugs.